Written by Kathleen Morrison
Medically Reviewed by Andrea Sleeth WHNP-BC, MSCP
Key takeaways
- Period headaches are common, showing up right before or during your cycle thanks to hormonal shifts, especially that pre-period dip in estrogen.
- Symptoms go beyond head pain and can include nausea, light and sound sensitivity, dizziness, fatigue, and trouble focusing.
- Hormone changes, stress, sleep patterns, hydration, and diet all play a role in how your headaches show up.
- Quick relief often comes from a mix of OTC options like ibuprofen or Excedrin, plus simple home strategies like ice packs, rest, and deep breathing.
- Paying attention to patterns in your cycle—tracking symptoms, meals, and triggers—helps you stay ahead and manage headaches before they take over.
- Hormonal options, supplements, and professional guidance through telehealth can give you more control and make headaches less disruptive.
If you get a period, chances are you’ve dealt with a headache or two (or ten). More than half of people who menstruate notice headaches around their cycle, ranging from a mild throb to full-on, can’t-even-get-out-of-bed pain. These headaches usually pop up right before or during your period, thanks to hormonal shifts, especially that pre-period drop in estrogen.
But period headaches don’t have to call all the shots. Once you understand what tends to trigger them and get a sense of what actually works for your body, you can take the edge off and feel more in control. Some people feel better with small lifestyle tweaks, others lean on specific treatments or preventive approaches, and most find it’s a mix that does the trick.
The goal is simple: help your body feel like itself again, instead of letting headaches hijack your day.
What is a period headache?
Period headaches, or menstrual migraines, are headaches that show up in sync with your menstrual cycle. These aren’t random headaches that happen to hit while you’re on your period; they’re triggered by the hormonal swings your body goes through each month, especially that pre-period drop in estrogen.
Where the pain happens
These headaches usually have a “signature spot.” Most often, the pain hits one side of your head, but it can hop sides or even settle on both at the same time. That throbbing sensation often starts at the temple and can spread across the forehead or sit right behind the eye.
The intensity varies, but menstrual migraines tend to be sharper and more focused than regular tension headaches. The affected area can feel super tender, so even laying your head on a pillow or gently brushing your hair can be uncomfortable.
Other common signs
Period headaches don’t just mess with your head, they can affect your whole body. Here’s what you might notice:
- Nausea: feeling queasy or even actually throwing up.
- Light sensitivity: even dim lighting can feel harsh.
- Sound sensitivity: everyday noises feel way louder than normal.
- Dizziness: the room might spin a bit or feel unsteady.
- Fatigue: beyond your usual period tiredness, feeling extra wiped out.
- Trouble concentrating: focusing on work or conversations feels harder than usual.
- Visual disturbances: some migraine patients see spots, flickers, or zigzag lines, though it’s less common with pure menstrual migraine.
These are your body’s subtle (or not-so-subtle) ways of telling you to slow down, rest, and take care of yourself.
Why do period headaches happen?
Getting why menstrual headaches show up helps make sense of why they hit some people harder than others and why they can feel so relentless.
Hormone changes in your cycle
Your hormones are doing a little dance every month, and sometimes your brain isn’t a fan. We can’t blame it.
Estrogen rises in the first half of your cycle, peaking just before ovulation, and then drops if pregnancy doesn’t happen. Progesterone also falls, with the sharpest dip right before your period starts.
For people prone to migraine headaches, this hormone drop is like flipping a switch for pain signals. Lower estrogen affects serotonin, the brain chemical that helps keep pain in check, so your nervous system gets extra sensitive and your blood vessels can react more strongly—hello, headache.
Other migraine triggers
Hormones set the stage, but a few other things can sneak in and make headaches worse during your period. Stress often spikes during PMS, poor sleep makes your brain more vulnerable, and dehydration (especially if your flow is heavy) can make a headache hit faster.
What you eat matters too. Cravings for chocolate, salty snacks, or even alcohol can introduce common migraine triggers. Blood sugar swings from skipped meals or changed eating patterns add another layer of headache risk.
It’s a lot, but knowing these factors can help you notice patterns and take charge of how you handle them.
How to manage a period headache
When a menstrual migraine shows up uninvited, quick relief becomes a must. Knowing your go-to strategies can make all the difference between hours of discomfort and getting back to your day. Treating menstrual migraines (and fast) usually needs a mix of smart medication choices and simple home tricks.
Over-the-counter medications
Some OTC options can help with menstrual migraine treatment:
- Ibuprofen (Advil) or naproxen (Aleve): Great for tackling both headache pain and menstrual cramps. Taking 400–600mg of ibuprofen at the first sign of a headache often works within 30–60 minutes. Keep in mind to always read the dosage instructions on your packaging—and remember you may need to wait a few hours in between doses.
- Excedrin Migraine: Combines acetaminophen, aspirin, and caffeine. The caffeine may help blood vessels contract and help boost pain relief.
- Midol Complete: Offers similar relief plus some extras for bloating and fatigue.
- Tylenol Extra Strength: A solid alternative if NSAIDs aren’t an option, though it may be less strong on inflammation.
Simple home remedies
Natural tricks can complement medications for some people to help them feel more comfortable:
- Cold therapy: Apply an ice pack or cold compress to your head, neck, or temples for 15 minutes to ease pain and inflammation.
- Dark, quiet space: Resting in a low-stimulation environment can help your body handle the headache better.
- Lie down and close your eyes: Even 20–30 minutes of this can make a noticeable difference.
- Deep breathing or gentle meditation: May help calm your nervous system and give you more control over the pain.
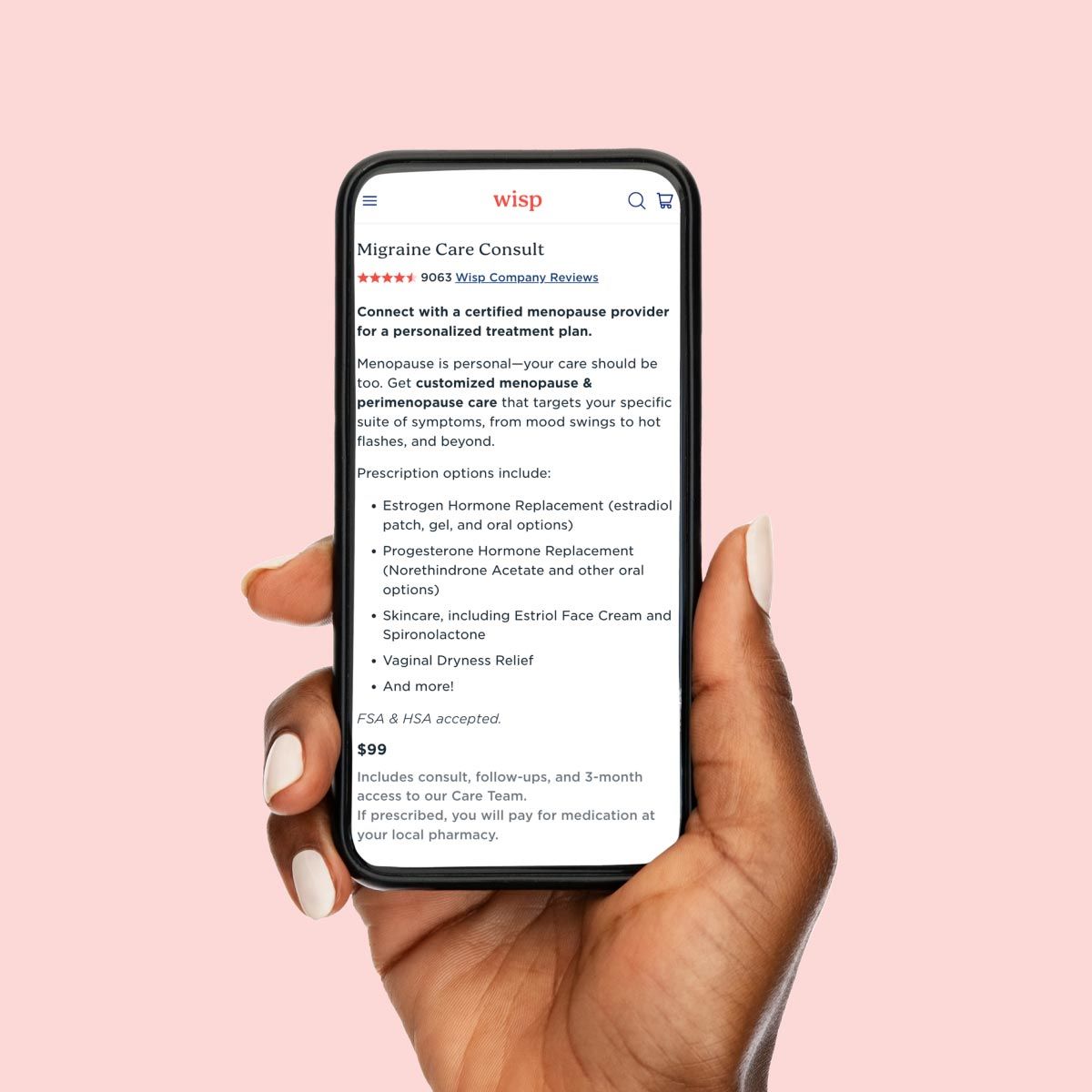
With an online migraine consult, a healthcare provider can help you decide what kinds of meds might work best for you to handle pain and help keep menstrual headaches and migraines away.
Can you keep period headaches away?
Period headaches might show up like clockwork, but there are ways to stay ahead of them. It all starts with tuning into your body and noticing patterns in your cycle so you can take charge before the pain hits.
Eating regularly and keeping your meals balanced with complex carbs and protein can help steady your blood sugar, which makes a bigger difference than you’d think.
Watch out for foods that may trigger discomfort for you in the days leading up to your period—this is different for everyone and may include things like overly processed snacks, caffeine, or certain sugary indulgences. But keep in mind that there’s no real research proving that any foods actually trigger head pain.
Some people find that supplements can be helpful too: magnesium glycinate, riboflavin (vitamin B2), CoQ10, and omega-3s can be beneficial for menstrual headaches.
Hormonal options can make a huge difference as well. Continuous combined oral contraceptives like Seasonique or Amethia keep hormones steady and skip the hormone-free interval that can spark headaches. Continuous vaginal rings, such as NuvaRing or EluRyng, do something similar. If estrogen isn’t an option—especially for migraine with aura—progestin-only methods like:
- Mirena or Kyleena IUDs
- Nexplanon implant
- Slynd
- …often make periods lighter or even disappear, which can keep headaches from showing up so often.
Hormonal birth control is a safe (and super common) way that loads of people with periods manage their symptoms, including headaches. So there’s no shame in it.
With these strategies in place, it’s about finding the combo that works for your body and staying consistent. A little planning and awareness goes a long way toward keeping period headaches at bay, so you can focus on living your life instead of letting the pain call the shots.
Wisp treatment options are available only after consultation with a licensed medical professional. You should consult with your healthcare provider before starting a new supplement or treatment regimen. Individual results may vary.
When to see a healthcare provider
It can be tricky to know when a period headache is just a monthly nuisance or something that deserves a professional check-in. If your headaches suddenly feel stronger, hit more often than usual, or just feel different from anything you’ve had before, it’s time to get it looked at. No guilt, no waiting it out.
Sometimes OTC meds aren’t enough, and a prescription can make a world of difference. Common options include:
- Triptans like Imitrex (sumatriptan) and Maxalt (rizatriptan) for stopping migraines in their tracks
- Perimenstrual Frova (frovatriptan) for targeted timing around your cycle
- Newer CGRP options like Nurtec ODT (rimegepant) or Ubrelvy (ubrogepant) for those who can’t take triptans
It’s also worth checking in with a healthcare provider if you’re having more than four headache days a month or if your headaches are interfering with work, school, or life. They might run blood tests to look at hormones, thyroid function, or rule out anything else going on.
Getting the right guidance can make a huge difference, and knowing when to reach out puts you back in control. You shouldn’t be guessing your way through every period.
Headaches don't call the shots
Period headaches might try to steal the spotlight every month, but they don’t have to run your life. Understanding your hormonal patterns and noticing your symptoms gives you the power to take charge of your cycle.
Finding what works often means trying a few things: hydration, steady sleep, OTC meds, or supplements can all help. Hormonal options and prescriptions might be game-changers, too, and getting professional guidance makes the process way less stressful. With Wisp, expert care is just a few clicks away, whether you need same-day birth control, migraine treatments, or a quick online consult.
Ready to take charge? Wisp makes it easy to get care on your schedule with fast, discreet delivery or same-day pharmacy pickup.
This blog post is for informational and educational purposes only and should not be taken as professional advice. Always consult with a qualified professional before making any decisions based on the information provided here.